Tooth decay is a widespread dental issue, affecting 26% of people in the United States with untreated cavities. If left untreated, tooth decay can manifest in various ways, including the development of a root canal infection. When it comes to treating such decay, many patients face the decision of choosing between Tooth Filling vs. Root Canal, Victoria Dentist TX.
Root canal therapy is a highly effective alternative to tooth extraction. It helps people preserve their beautiful smiles with minimal inconvenience. However, while root canal therapy has significant benefits, it’s often perceived as a painful procedure, making some patients apprehensive. Given this, a common question arises: is a dental filling a reasonable alternative to a root canal?
Is a Dental Filling a Viable Substitute for Root Canal Therapy?
Although fillings are categorically less radical than root canals, most patients prefer fillings to root canals. However, the degree of infection decides whether a dental filling is appropriate or a root canal. If the decay has spread to the pulp, then the treatment is root canal treatment. However, a filling may be enough if the affected tooth has residual decay or a small cavity that has not reached the pulp.
It is also important to pay attention to the tasks that these treatments accomplish. Whereas root canal treatment is needed to stop further decay as it works on the infection of the pulp of the tooth, a dental filling is mostly centered on the need to repair and make the tooth functional and cosmetically appealing again.
Can You Get a Filling Instead of a Root Canal?
Dental caries is one of the most common diseases of the oral cavity and 26% of the population of the United States has untreated tooth decay. If the decay is left untreated it can worsen and cause infection to the root canal. As a patient, a person is faced with two choices which are Tooth Filling or Root Canal, Victoria Dentist TX.
Root canal therapy is a highly effective way to preserve natural teeth and avoid extraction. It allows patients to maintain their smiles without significant hassle. However, despite its benefits, root canal therapy often carries a reputation for being painful, which can make patients hesitant. This brings up a frequent question: is a filling a suitable alternative to a root canal?
When Is a Dental Filling an Option over a Root Canal?
A dental filling is usually more straightforward and is generally more popular among patients because it is less invasive. However, the decision of whether to fill the tooth or to have a root canal depends on how far the decay has progressed. If the disease goes down to the tooth’s pulp, which contains nerves and blood vessels, the patient requires a root canal to eliminate the infection and preserve the tooth. If the decay is thin or localized in a pit that has not reached the pulp chamber, a filling is adequate.
The goals of these treatments are distinct. Root canal therapy targets infection within the pulp to prevent further damage, while a filling is focused on restoring a tooth’s function and appearance.
Understanding the Differences: Root Canal vs. Filling
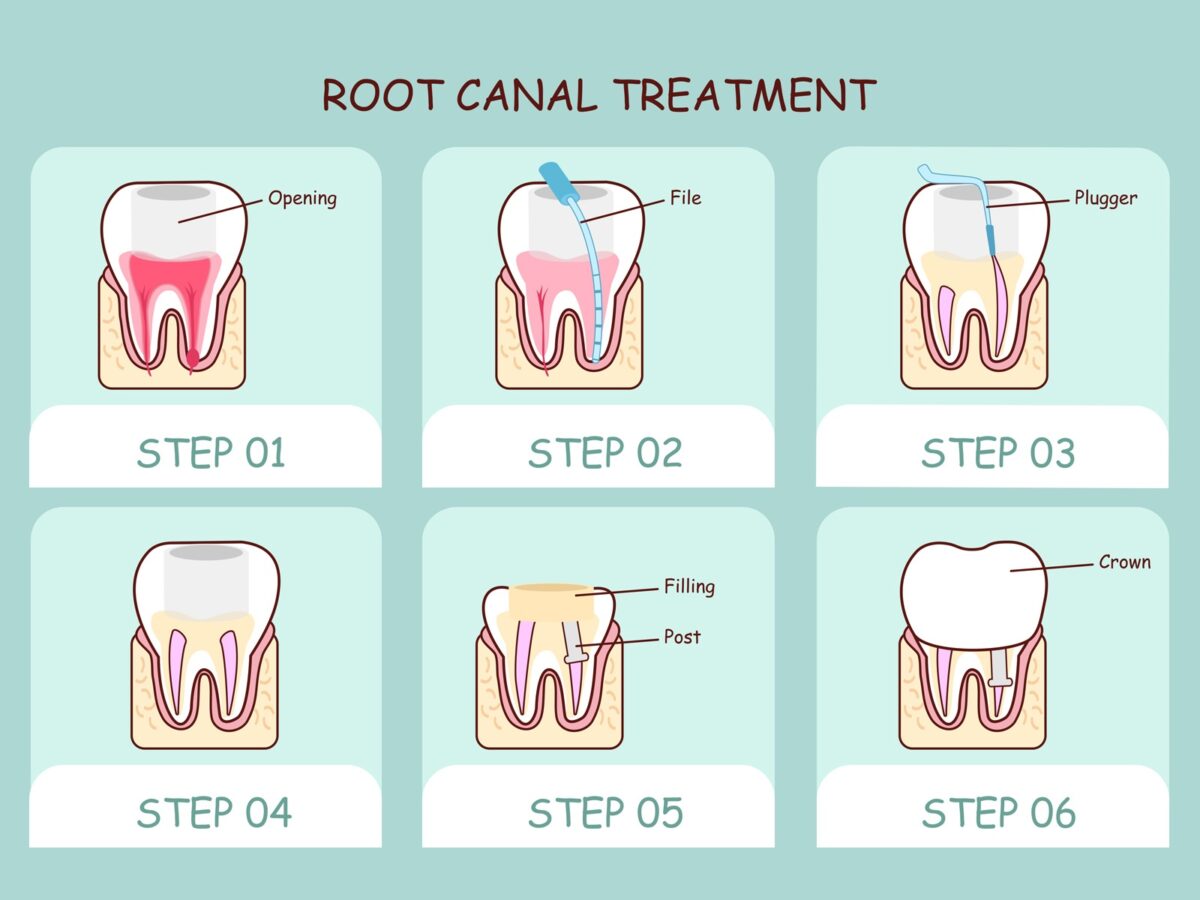
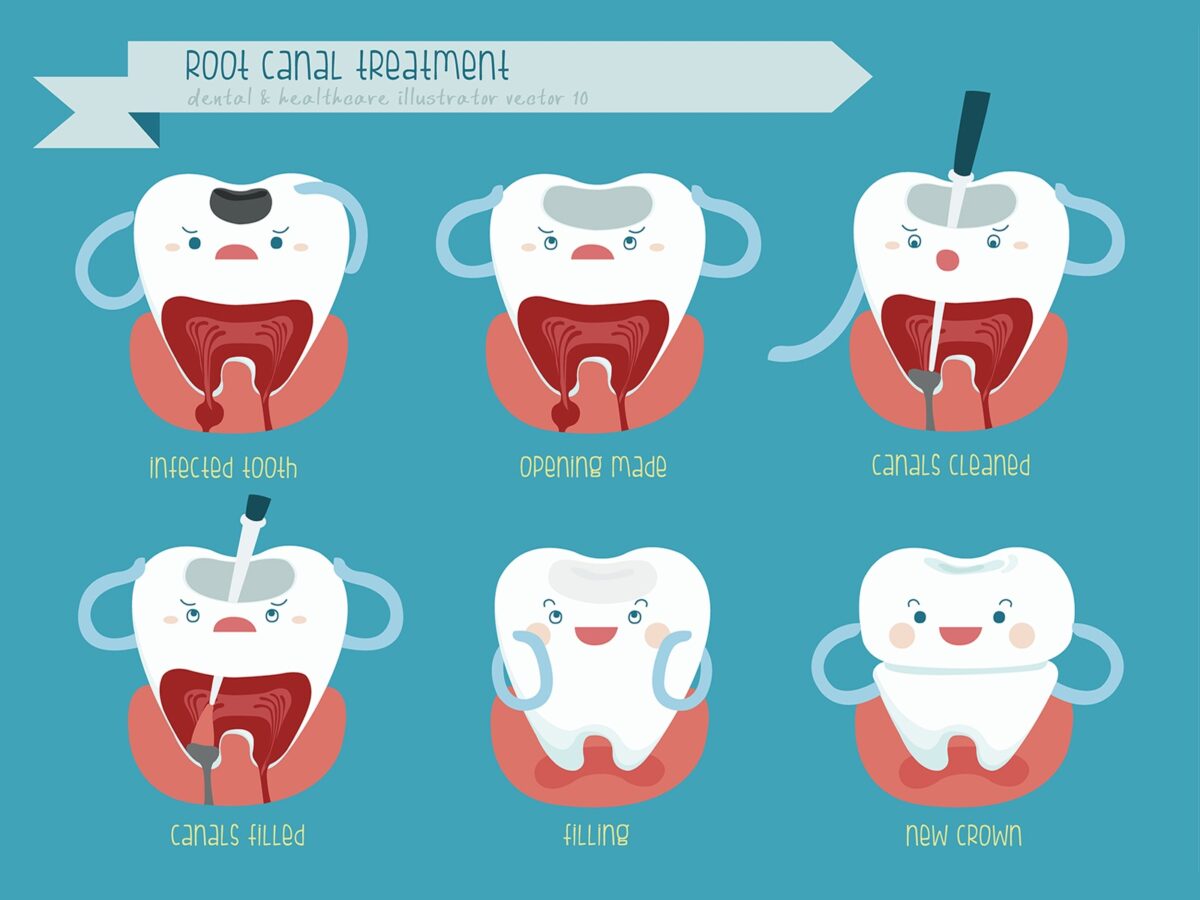
During a root canal, the dentist removes infected tissue from within the tooth, cleans and shapes the inner chambers, and seals it to prevent further infection. This approach saves the natural tooth, which is essential for preserving alignment and overall dental health. Meanwhile, in a filling procedure, the decayed area is removed, and the remaining space is filled with composite resin, amalgam, or gold. Fillings are typically faster and require minimal recovery, making them suitable when decay hasn’t impacted the tooth’s pulp.
Preventing the Need for Fillings and Root Canals
With the right preventive care, the need for either a Tooth Filling vs. Root Canal, Victoria Dentist TX can often be avoided. Maintaining proper oral hygiene, like brushing twice daily, flossing, limiting sugary foods, and scheduling regular check-ups with your Victoria Dentist TX, is crucial for keeping decay at bay.
Conclusion
In the end, whether a root canal or filling is recommended depends on the extent of the tooth decay. Root canals are necessary when the decay reaches the tooth’s pulp, whereas fillings are ideal for minor cavities. A consultation with a Victoria Dentist TX will help you decide the best treatment plan—Tooth Filling vs. Root Canal—based on your unique dental needs. Don’t hesitate to seek an evaluation to ensure long-term health and comfort for your smile.
Don’t delay your dental care—schedule your appointment with a Victoria Dentist TX to discuss Tooth Filling vs. Root Canal and get timely treatment!